Treatment of Keratoconus
What you will read...
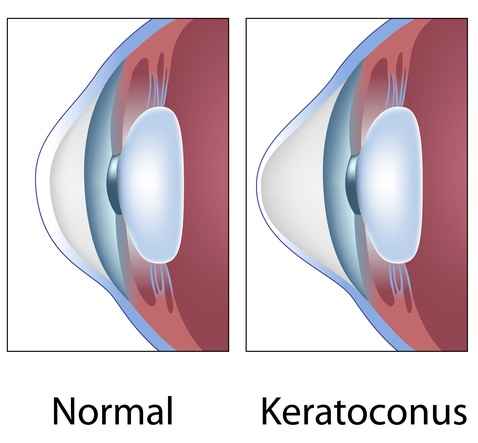
What is Keratoconus?
Keratoconus is a non-inflammatory condition that typically affects the cornea of both eyes. In this disease, the cornea becomes thin and takes on a conical shape. The thinning and change in the corneal shape from spherical to conical lead to the development of nearsightedness (myopia), irregular astigmatism, and, consequently, a decrease in vision. Keratoconus is a progressive condition that usually manifests during adolescence and progresses until the third or fourth decade of life when it often stabilizes. It typically starts in one eye initially but usually affects the other eye after some time, although the severity may differ between the two eyes. Keratoconus is a relatively common condition, observed in all races and in both genders. There is a family history in 6 to 10 percent of affected individuals.
causes of Keratoconus
Despite extensive research, the cause of keratoconus is still not fully understood. While this condition is not hereditary, rigorous eye rubbing, though not the cause of keratoconus, is not irrelevant to its development. Therefore, patients with keratoconus are advised to avoid rubbing their eyes.
Symptoms of Keratoconus
The clinical symptoms of keratoconus vary depending on the severity of the condition. As mentioned, this disease leads to a decrease in vision due to the induced nearsightedness and astigmatism, prompting individuals to seek the advice of an eye specialist. In the early stages, vision may improve with eyeglasses, but due to irregular astigmatism, it may not be corrected to 20/20 vision. In such cases, diagnostic tests such as corneal topography, aberrometry, pentacam, or other imaging methods are used to confirm the diagnosis.
Treatment of Keratoconus
For the treatment planning of each patient, a comprehensive ophthalmological examination and corneal imaging are necessary. In general, the treatment of keratoconus will be tailored to the severity of the condition and the patient’s overall eye health, and it will be accomplished through one method or a combination of the following approaches:
A- Use of glasses
In the early stages of the disease, the prescription of eyeglasses by an eye doctor can significantly improve vision. However, it should be noted that keratoconus is a progressive condition, and as a result, the prescribed eyeglass prescription may change over time.
B- Prescription of contact lenses
With the progression of the disease and the increase in nearsightedness and irregular astigmatism, there comes a stage where vision cannot be corrected with eyeglasses, and hard contact lenses are required to improve vision.
C- Use of ultraviolet (UV) or Collagen Cross-Linking (CCL or CXL) therapy
One fundamental challenge in diagnosing keratoconus is that in its early stages, the disease is somewhat covert and doesn’t pose significant problems. However, it gradually progresses over time, leading to serious visual disturbances. In the initial stages of the disease, the patient’s only issue may be the need for frequent changes in eyeglass prescriptions, double vision, halo effects, or light sensitivity. But as the disease advances and corneal irregularities worsen, the individual’s vision will progressively deteriorate.
This new treatment approach, known as Collagen Cross-Linking (CXL), utilizes ultraviolet light and riboflavin to strengthen the corneal collagen fibers. CXL has been a breakthrough in preventing the progression of keratoconus and has raised new hopes for patients. It is primarily aimed at halting the progression of the condition, and in more than 70% of cases, it can improve vision with or without eyeglasses.
D- Implantation of intracorneal rings
Another surgical treatment for keratoconus involves the use of intracorneal rings. This treatment is suitable for some cases of mild to moderate keratoconus where patients cannot tolerate contact lenses. These rings help improve vision by reducing irregular astigmatism. It’s important to note that the success rate of intracorneal rings varies significantly from one individual to another, and in cases where the treatment is unsuccessful, the patient may eventually require a corneal transplant.
The results of this procedure in keratoconus patients can be variable. On average, placing intracorneal rings can lead to an improvement of two lines of vision in half of the patients, although some individuals may experience more remarkable improvements. In fact, for keratoconus patients, this procedure can provide those who had poor vision with eyeglasses before the surgery with better vision after the rings are placed due to the reduction in corneal irregularities. However, it is not suitable for every patient.
E- Implantation of intraocular lenses (IOLs)
In patients with keratoconus who mainly have severe nearsightedness and minimal astigmatism, it is possible to correct the refractive error without removing the natural eye lens by implanting a specific intraocular lens (IOL) inside the eye. With this procedure, as the natural lens remains untouched, the eye’s ability to accommodate is preserved, and individuals who haven’t reached presbyopia age will have both good distance and near vision. In this procedure, a very small incision is made in the cornea to insert a thin lens in front of the natural lens to correct the refractive error caused by keratoconus.
These intraocular lenses come in various types. Some are positioned in the anterior chamber of the eye (behind the cornea and in front of the iris), while others are placed in the posterior chamber (on top of the patient’s natural lens and behind the iris). These lenses are permanently implanted inside the eye, but they can be removed through surgery at any time. Each type of lens has its own advantages and disadvantages. The foldable or flexible type of these lenses (Artiflex & Veriflex) is preferred for correcting severe nearsightedness. For cases with significant astigmatism, the toric type of these lenses is used. The advantage of these lenses is that they are inserted in a folded state and then opened inside the eye, allowing for a smaller incision and, consequently, less astigmatism caused by the incision.
F- Corneal transplant (keratoplasty)
In cases where the disease progresses further, there comes a stage where even the use of contact lenses or intracorneal ring segments does not provide an improvement in vision, and the corneal irregularities make it impossible to tolerate contact lenses. In this stage, a corneal transplant is necessary to address the vision problems.
Does keratoconus lead to blindness?
Fortunately, keratoconus is not a blinding disease, but it is one of the common reasons for corneal transplantation. Individuals with keratoconus or their relatives should not be overly concerned because the disease is relatively benign, and corneal transplantation can be successful in improving vision.
